Vertebral Compression Fractures and What Can Be Done About Them
You might not think so, but your skeleton is a remarkably active vital organ. It serves two necessary functions in your body: structure and storage. Structurally, bones protect your other organs. They create a framework for muscles and tendons that allow us to move. As a storehouse, bones stockpile essential minerals. This ensures they are available when needed. These minerals (mostly calcium) make it possible for the heart to beat; muscles to contract; nerves to conduct impulses; and other bodily processes. We need steady blood levels of calcium at all times. If one system is running short of calcium, the signal goes out requesting more. If there is not enough in circulation, calcium is taken from your bone storehouse. This doesn’t cause any harm if it happens once in a while. However, too many withdrawals can lead to osteoporosis and easily broken bones. This type of broken bone is called a “fragility” fracture because it happens in very weak bone under conditions that would not break normal healthy bone.
What Is a Vertebral Compression Fracture (VCF)?
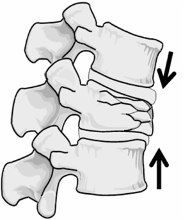
Your spinal column has 33 small bones (vertebrae) stacked up from skull to tailbone. Vertebrae protect your spinal cord, support your head, and attach to muscles and tendons so you can move. Normal vertebrae are shaped a bit like marshmallows. Inside, they are filled with a branching honeycomb of tiny connected bones. Bones in your spine are rich in calcium and other essential minerals. If your body is running short of these minerals, they are taken from vertebral bone. The honeycomb gets thinner and weaker. The connecting branches break. When enough bone is lost, cracks form and the vertebra collapses. This is called a vertebral compression fracture (VCF). Most of the time, vertebrae collapse toward their more heavily loaded side. This creates a wedge shape that shifts spinal load forward or to one side. Shifting more weight onto other vertebrae makes them more likely to collapse as well. And they do. The majority of people have a second VCF within a year of their first one.
Why Do You Need to Know About VCF?
Vertebral compression fractures are often painless. Even when you don’t feel a VCF, its potential impact is serious. Risk for death goes up 15% in the six months following a vertebral fracture.
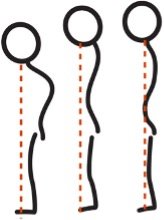
By slightly changing how weight is balanced on the spine, each broken vertebra raises the risk for another. These VCFs may not be discovered until extreme curvature of the spine has developed (so-called “dowagers hump”).
Spinal curvature gets progressively worse the more VCFs you have. Pain develops in back and chest muscles that have to work extra hard to hold you upright. It gets harder to walk, stomach troubles develop, breathing gets difficult. If nothing is done, disability and loss of independence often result.
Most VCFs can be prevented. Even when you have had more than one, you can lower your risk for more. The key to prevention is knowing your risk. Once you know, you can take preventive action.
How Do You Know If You Have a VCF?
Sometimes it is obvious that you have a VCF. You swing your tennis racket and suddenly have a sharp pain between the shoulder blades. If the pain gets better when you lay down and worse when you stand up, it may be a VCF. This type of VCF can be very painful. An x-ray or other scan can confirm the VCF and its severity. Your healthcare provider will likely prescribe a short period of rest, back bracing for support while the bone heals, and painkillers to keep you comfortable. Too much bed rest is very bad for bones and general health. However, your bones need rest to heal. Even when you are back on your feet, rest will be important. Taking short breaks throughout the day will keep pain from getting out of hand. If your pain continues after 4-6 weeks or is intolerable, talk with your doctor. There are treatments that can help (see Treatments below).
What Is a Silent VCF?
Most of the time, VCFs occur without any injury or pain. These “silent” VCFs can be caused by something as harmless as a sneeze. You won’t even notice. One of the first signs that a person has had silent VCFs is height loss. It can be easy to miss gradual changes in height loss. Ask yourself:
Have you noticed that ….
... Pants you have worn for years need hemming?
... Adult children seem to be getting taller?
... It is harder to reach the upper shelves?
If your answer is “yes” to any of these questions, you have probably lost an inch or two. This may indicate a silent VCF. It means you need to take steps to avoid more.
What Should You Do if You Have a VCF?
If you suspect that you have had a VCF, talk with your doctor. You will probably be referred for X-ray, MRI, or other type of scan. Healthy vertebral bones don’t break without serious injury. Osteoporosis is almost always the cause. Osteoporosis doesn’t get better without effective treatment. Your next step is very important. Preventing more broken bones will depend on you.
Treatments for VCFs and Prevention Strategies
Popular media would have us believe that—on their own—diet and exercise can cure osteoporosis. It is easy to see why. Most people do not want to take medications, and certainly not medications that have been linked (again in the popular media) to scary side effects. What the media doesn’t point out is that VCFs are extremely common, while these drug side effects are extremely rare. It’s like getting struck by lightening twice. Of course, good nutrition and exercise are critically important. They just aren’t enough. Effective anti-fracture treatment is needed as well.
What Medications Can Help Prevent VCFs?
There are many medications on the market proven to preserve bone in people with osteoporosis. These drugs reduce the likelihood of having a fragility fracture. You have your choice of daily, weekly, or monthly tablets, daily injections, yearly IV infusions, and other options. There is no best medication for everyone. The one that works for you depends on many factors. Your health history and preferences are considerations. Talk it over with your doctor.
How Can Diet and Nutrition Help?
Whatever medication you are prescribed for osteoporosis, it won’t work without enough calcium and vitamin D. Most people can get the calcium they need from foods like cheese, yogurt, and fortified cereal. Calcium tablets are good for filling in when you can’t get enough in your diet, but it is always better to get calcium from food. Still, calcium by itself is not enough. You also need enough vitamin D. Without vitamin D, your body can’t absorb calcium from food. Getting enough vitamin D can be difficult. Vitamin D is naturally made by bare skin in reaction to sunlight. Many people get too little sun or have skin that doesn’t absorb much vitamin D. This is the case in older adults and darker skinned people. Sunscreen and sunblock also prevent the skin from making vitamin D. For these individuals, extra effort is needed to avoid bone damage. Because there aren’t many food sources of vitamin D, supplements are recommended for people who need them.
How Can Physical Therapy Help?
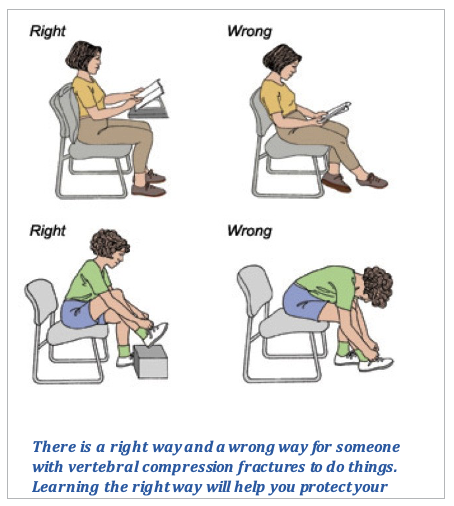
Following a VCF, physical therapy (PT) will be an important part of your recovery. Physical therapy for VCF focuses on relieving pain and reducing risk for another fracture. You will learn spine-safe posture, body dynamics, and exercises to improve balance, strength, and stamina.
To prevent future fractures, you will probably need to learn new ways to perform tasks of daily life. Things like sweeping and carrying groceries can break a bone if not done mindfully. Proper alignment is key to safe movement. Lining up your head, shoulders, spine, hips, knees and ankles improves balance and centers weight over your legs. Certain positions and movements are dangerous for people with fragile spinal bones. These include: slouching; forward bending and twisting; motions that are abrupt or jarring; and lifting heavy objects, either from the floor or from overhead. More information on safe movement can be found in BHOF’s Boning Up on Osteoporosis booklet, available on the BHOF website.
What Exercises Should Be Avoided?
Keeping active is absolutely necessary for good health and longevity. However, for people with VCFs or osteoporosis, some exercises can do more harm than good. If you have low bone density, osteoporosis, or spinal curvature, you should avoid exercises that involve bending over from the waist, such as:
• Sit-ups
• Abdominal (stomach) crunches
• Toe touches
• Squats
If you have one or more VCFs, you may need to make changes to your recreational activities. Yoga, Pilates, tennis and golf involve twisting and bending motions that can overstress weakened spinal bone. If you have VCFs, it’s also a good idea to avoid anything that could result in a fall, a hard bump, a fast stop, or a severe twist. Horseback riding, ice hockey, and gymnastics would likely be out. On the other hand, golf might be okay with the right changes to your stroke. Work with a physical therapist or trainer to ensure spine safety.
Why Is Preventing Falls So Important?
Falls are the leading cause of broken bones in older people. If you prevent falls, you prevent most fractures. Many factors contribute to falling in older people. These include bad eyesight, balance problems, weak legs, dizziness, and slow reflexes. A lot can be done to reduce risk for falls. Keep your glasses prescription up to date. Work with your physical therapist on muscle strengthening and balance training. Let your doctor know right away if you are feeling dizzy. Dizziness is a common side effect of many medications and illnesses. Stay as active as possible to build endurance and agility.
Homes and workplaces can be made safer. Take an inventory of your environment. Get rid of loose rugs, slippery surfaces, and tripping hazards. Make sure there are grab bars in your bathroom and strong handrails on your stairs. Put in brighter lights, especially outdoors and in stairways. Professional home safety experts can help with assessment, selection, and installation of any needed features.
What Can Be Done for Severe VCF Pain?
Most patients with VCF feel better after a couple weeks of rest, bracing, and pain relievers. However, some VCFs cause extreme pain that persists. In these cases, there are options to consider. You may be able to get better pain control working with a physician who specializes in pain treatment. You may get relief using a combination of medicines and physical treatments such as acupuncture or massage. Sometimes a VCF is still unbearably painful after a month of rest, medication, and physical therapy. Your doctor might refer you for further evaluation. In some cases, surgery may be recommended.
When a vertebral bone is broken, fragments of bone can rub against one another, causing intense pain. Keeping these fragments from moving usually relieves the pain. An operation called vertebral augmentation is designed to do just that. Vertebral augmentation is called a “minimally invasive” surgery because it involves relatively less operation time and less recovery time. Unlike a major surgery, only one or two small openings are needed in the skin. Bone cement is injected through a needle into the crushed vertebra. Once the cement hardens, the bone fragments are cemented in place.
There are two types of vertebral augmentation: vertebroplasty and kyphoplasty. Both use bone cement to stabilize broken vertebral bone. The difference is that in kyphoplasty the crushed vertebra is expanded using a balloon. This creates more space for cement and pushes the bone upward, returning it to a more natural shape.
Vertebral augmentation is covered by many health insurances; however, you should confirm this with your particular insurance company.
Summary
A strong adult skeleton starts in childhood with optimal diet, exercise, and sunshine. Even if you don’t achieve your full skeletal potential, fractures can be prevented. Universal recommendations for bone health include adequate vitamin D and calcium, weight-bearing exercise, and avoidance of smoking and excess alcohol intake. Additional fracture preventive measures may be needed. If you have had previous fractures, have a family history of fragile bones, or have been diagnosed with osteoporosis, you and your healthcare provider should discuss options for effective anti-fracture treatment.
Traditional first-line management for VCF focuses on bed rest, bracing, and pain control. While effective for most, pain persists in some patients. For individuals experiencing severe pain after four to six weeks of conservative management, minimally invasive vertebral augmentation can offer hope for improvement.
For additional information, visit the BHOF website at bonehealthandosteoporosis.org. There you will find newsletters, handbooks on exercise and safe movement, ant-fracture medications, access to support groups, and more.
To download and print the original PDF brochure from the Bone Health and Osteoporosis Foundation website, please click here.