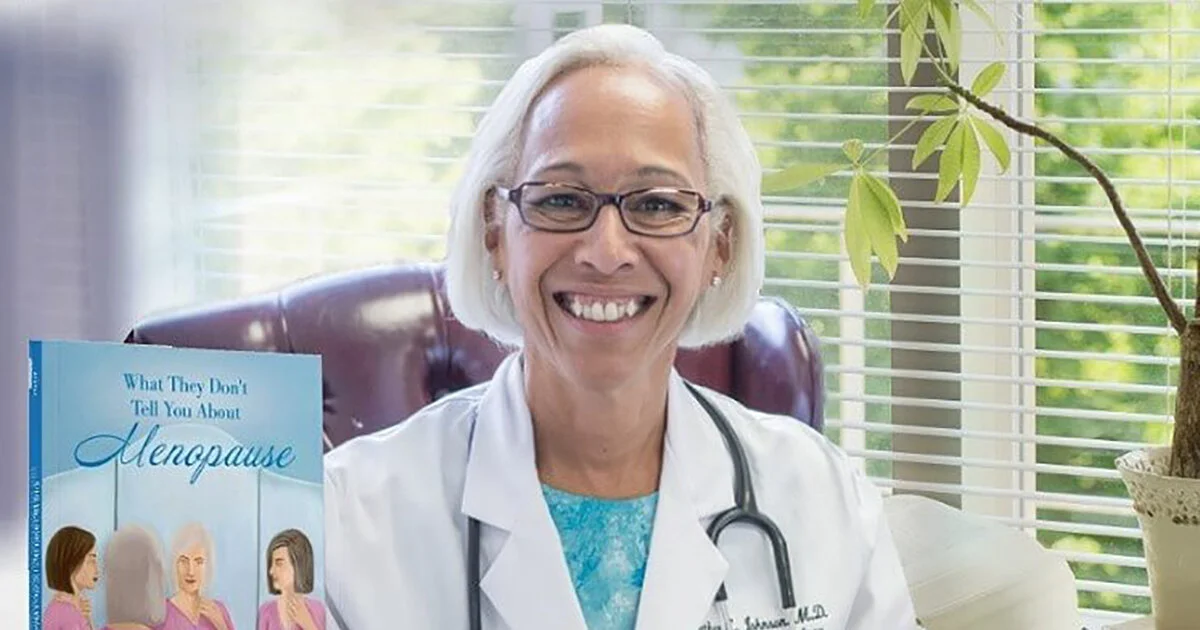
Guest Post By Dr. Heather Johnson
Dr. Heather L. Johnson is an actively practicing gynecologist and author of two books about pregnancy and menopause, who, after delivering more than 3,500 babies over 40 years, recently retired as an obstetrician.
What is osteoporosis?
Osteoporosis is a skeletal disorder caused by loss of bone mass, or density, that results in deterioration and fragility of bone leading to an increased risk for fracture from minor trauma.
What causes osteoporosis?
Bone is active, living tissue that builds, rebuilds and reshapes itself during our lifetime. Cells called osteoclasts rebuild damaged bone. Cells called osteoblasts break down damaged bone. Prior to the age of 30, there is a net gain in bone mass/density. After that, there is a slow decrease over time. Family history, genetics, gender, lifestyle and certain medical conditions affect the peak bone density and the speed with which this density is lost.
What are risk factors for developing osteoporosis?
Postmenopausal status (see below) is the biggest risk factor for developing osteoporosis. Those with a family history of osteoporotic fractures, females, and Caucasians have a higher risk of developing osteoporosis as do smokers. Individuals treated long-term with corticosteroids (such as prednisone for disorders like asthma or various autoimmune disorders like lupus or rheumatoid arthritis) are at an increased risk of developing osteoporosis, as are women who have prolonged episodes in their reproductive lives without menstrual cycles including anorexics, those taking a hormone called Depo-Provera for period or birth control, elite athletes, and women with premature ovarian failure.
How does menopausal status affect the risk for developing osteoporosis?
Technically speaking, a woman is menopausal a year after her last menstrual period. From that point forward, she is postmenopausal and no longer produces estrogen in any meaningful amount.
The loss/decrease of estrogen in the menopausal period results in a decrease in bone density by accelerating the age-related loss in bone mineral density. There is a rapid change in the first 5-7 years after the last menstrual period making individuals who enter this period more likely to develop osteoporosis.
Can bone loss be prevented or decreased?
Absolutely. While one cannot control factors such as ethnicity, gender, and family history, we can adopt lifestyle changes to promote healthy bones. If you smoke, stop!
Diet: Provide your body with the building blocks for making bone, i.e. calcium and protein. For most, protein is easy. For many, calcium is not. Prior to menopause, women need 1,000 mg of calcium a day. After menopause, the amount is 1,200 mg. Dairy products are the best source (e.g., milk, cheese, yogurt), and 3 or more servings a day will provide what you need. If you cannot or prefer not to consume these products, many milk substitutes, such as almond milk, have added calcium as do fortified breakfast items (e.g., cereals, juices, breads). Be sure to check the label. While a number of vegetables are high in calcium, for vegetables, it might require eating 10 cups of broccoli or half a pound of parsley a day to get the required amount. Over the counter supplements are available for what your diet does not provide. Please note that the body can only absorb 500-600 mg at a time so taking the entire amount at one time is not helpful.
Vitamin D is necessary for the absorption of calcium. If you take supplements, consider those that contain this vitamin as well. The recommended daily allowance of vitamin D is 400 to 800 IU. Although sunlight is often recommended to increase your level, sunscreen will limit the benefits, and avoiding sunscreen is not recommended.
Exercise: Regular weight bearing exercise is essential to maintaining bone health. This means a minimum of 20-30 minutes 3-5 times a week. Exercises include walking (with or without weights), running, aerobic machines, strength training, yoga, Pilates, pretty much anything but swimming, which is not weight bearing, will do. Activities such as tai chi and yoga help improve balance and affect your awareness of self in space to prevent falls.
Fall-prevention at home: Falls can be a game changer, so it is essential to take the time to fall-proof your house sooner rather than later! Easy ways to start to “fall-proof” your home include: covering electric cords, removing or securing throw rugs, providing night lights for those inevitable nocturnal trips to the bathroom, and monitoring medications that cause sedation.
How do I know if I have bone loss?
A simple bone density X-ray called a DEXA scan can tell you if you have age-appropriate bone loss known as osteopenia, or pathologic bone loss known as osteoporosis. The recommended age for getting this test is 65, but those who are at higher risk than average should consider getting tested after they have become menopausal.
What medications are available to treat/prevent osteoporosis?
HRT: Hormone replacement therapy (HRT) taken for treatment of severe menopausal symptoms presses the “pause” button on the development of bone loss. At some point though, most women stop taking these medications for symptoms and will need to refocus their efforts at maintaining bone health.
Prescription medications: Oral medications that change the balance between bone building and breakdown of bone are available and do a very good job in high-risk individuals. There are side effects, as with any medication, but for women with significant loss, these side effects pale in comparison to the detrimental and long-term effects of a hip fracture.
Speak with your gynecologist, internist or endocrinologist about these options.
ABOUT
Dr. Heather L. Johnson is an award winning, actively practicing gynecologist AND author of two books about pregnancy and menopause, who, after delivering more than 3,500 babies over 40 years, recently retired as an obstetrician. In her second book, What They Don’t Tell You about Menopause: A Gynecologist’s Unofficial Guide to Premenopausal, Perimenopausal and Postmenopausal Life, she discusses the various stages of menopause and what to expect throughout this natural aspect of life for women. From perimenopause to postmenopause, and everything in between, this book offers practical, fact-based information that will be your guide through this daunting period of womanhood.
In both of her books Dr. Johnson shares what she has learned throughout her career, fact-filled and up-to-date medical insights, humorous anecdotes, and “Dr. J’s Pearls” of bite-sized advice & information. Her books are available in both Paperback and eBook on Amazon.com, BarnesandNoble.com, Walmart.com and Goodreads.com.
She is the senior partner at Reiter, Hill & Johnson, an Advantia practice, with offices in Washington, DC, Chevy Chase, MD and Falls Church, VA. Dr. Johnson attended Yale University School of Medicine and trained at The Walter Reed Army Medical Center in Washington, DC. She has two children and is a proud grandmother of two granddaughters.
To learn more about Dr. Johnson, her books and Dr. J’s Pearls of bite-sized advice, please visit her website https://AskDrHeatherJohnson.com, and follow her on Instagram (@askdrheatherjohnson), Facebook (@askdrheatherjohnson) and Twitter (@askdrjohnson)!